The term free-floating thrombus (FFT) is not exact because they are attached to the vein wall by a base and not actually “free”. A true free thrombus is termed an embolism. A FFT within the veins of the leg represents a potentially serious situation. Detachment can cause travel into the deep veins and then into the lungs. This is termed a pulmonary embolism (PE) which may be fatal if it causes an acute arrest of the pulmonary circulation. If the thrombus burden is small, for example if only part of the thrombus detaches, then the patient may survive. Frequent and multiple PE may cause pulmonary hypertension from the fibrosis and thickening to the pulmonary arteries in response to the thrombus. In reality, once the diagnosis of FFT has been made the outcome is not as originally supposed.
TAKASHI YAMAKI Most published guidelines for treatment of acute and subacute deep vein thrombosis (DVT) recommend early ambulation over initial bed rest. According to the recent guidelines of the American College of Chest Physicians (ACCP), pharmacological treatment has been recommended for patients with confirmed acute deep vein thrombosis (DVT). For patients with acute DVT, early ambulation is recommended over initial bed rest. Furthermore, inferior vena cava (IVC) filters are recommended only if anticoagulation is contraindicated. These recommendations suggest that the existing guidelines tend to be applicable to thrombi that are firmly attached to the vein wall. On the other hand, the FFT represents a particular form of DVT that is considered to carry a high risk of fatal pulmonary embolism during ambulation. Therefore, the management of FFT in the femoro-popliteal or ilio-femoral veins is controversial. Furthermore, the accurate incidence of FFT among patients with acute DVT and the natural history of FFT in this population are not well understood.
Depending on various evaluation methods, the prevalence of FFT in the proximal deep veins has been reported to range from 6% to 59%. Approximately, 50% of patients with confirmed PE have concomitant DVT as a source of PE. As FFT is considered to carry a high risk of fatal PE, decisions on the prophylactic use of IVC filters for these patients are made on a case by case basis. However, a large randomized study revealed that use of IVC filters did not improve the rate of mortality due to PE in patients receiving anticoagulation relative to those receiving anticoagulation alone. Therefore, the existing guidelines do not consider FFT to be an indication for insertion of IVC filters.
The fate of FFT during anticoagulant therapy has not been well investigated. Our results showed that FFT became attached to the vein wall in 43% of the patients within a mean of 9.3 days and that FFT resolved spontaneously in 57% of the patients within a mean of 19.3 days without any further thromboembolic complications. This indicates that PE usually occurs before a diagnosis of FFT is made. Therefore, the fate of FFT is can be largely divided into attachment of the thrombus to the vein wall with subsequent recanalization or spontaneous resolution.
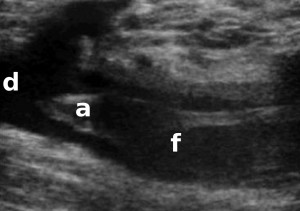
Ultrasound image of the apex (a) of a free-floating thrombus (f) within the femoral vein. This has the potential to detach into the deep veins (d) and travel into the chest causing a pulmonary embolism.