Traditionally the management of a deep vein thrombosis (DVT) was easy and straight forward. Patients diagnosed would receive a short course of intravenous heparin followed by oral warfarin. The warfarin would be continued for 6 months. Compression stockings were advised and prescribed in most circumstances. Within the last 10 years the management of DVT has become increasingly invasive. There is accumulating evidence that this invasive approach may reduce the amount of valve damage from the DVT and prevent many patients from developing the post-thrombotic syndrome. The overriding principal governing the change in practice is that the earlier the DVT is resolved the greater the reduction in valve damage and thrombus organisation into fibrosis.
GERARD O’SULLIVAN The treatment of acute proximal DVT remains controversial. In selected patients we believe that a quin-tuple therapy approach is required. This involves direct chemical thrombolysis via an infusion catheter with tissue plasminogen activator (tPA), mechanical thrombus disruption using a revolving/vibrating wire or other device, balloon angioplasty of provoking/remaining lesions, venous stenting and the application of intermittent pneumatic compression to both legs. Recently we treated a long distance runner in this way who presented with a 5 day history of a grossly swollen left leg. She had a May-Thurner iliac vein compression which may have precipitated her initial DVT. This was accessed using a 10 Fr sheath via the popliteal vein in the prone position. After pharmaco-mechanical thrombolysis the provoking compression was treated by balloon venoplasty and stent deployment across the lesion. Duplex imaging the following day revealed a widely patent stent and veins. The patient resumed her running distance of 10 kilometres per day. This technique may be the preferred approach in most patients presenting with a proximal DVT.
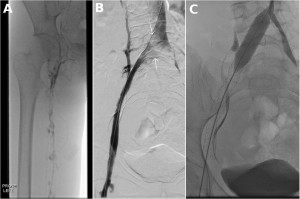
Sequential images in the prone position. Acute left ilio-femoral DVT (A), pharmaco-mechanical thrombolysis reveals pancaking of the left common iliac vein (B, arrows), venoplasty and stenting of the left common/external iliac vein (C).