Venous ulcers are an infrequent complication of prolonged venous hypertension and are a considerable burden to health resources. Approximately 10% are painless and do not interfere with the patient’s quality of life. Treating the superficial venous reflux often results in a cure but re-ulceration is possible in the absence of interference from deep axial reflux and/or perforating vein reflux. The causes of venous ulceration are multi-disciplinary and multi-factorial.
FIRMILIAN CALOTĂ Venous leg ulcers (VLUs) are chronic skin lesions characterised by a loss of substance in the soft tissues, scarring, lipodermatosclerosis and exudation. The cause is often a complex interplay of factors. These are best illustrated as a Venn diagram with multiple intersecting components. The predominant component of all generic ulcers usually classifies them. For example: venous, arterial, arthropathic, neuropathic, post-thrombotic, malignant, mixed and dependent. This may have the consequence of ignoring other treatable components.
All VLUs have a primary venous component by definition. The primary function of veins is drainage. Drainage insufficiency can be caused by reflux, obstruction, loss of venous tone and pumping insufficiency. Secondary components are frequent and include arterial ischaemia, arthropathic conditions with a reduction in mobility, and obesity. Failing muscle pumps like the heart and calf muscles may contribute to a reduction in the venous drainage. The consequence of all this is venous hypertension with a persistent and prolonged pressurisation of the connecting tissues. Pressure and time leads to inflammation, damage and scarring. Eventually a VLU may develop.
Venous pressurisation leads to activation of leukocyte producing cytokines, macrophages and collagen-secreting fibroblasts. Fibrous tissue is an inheritant part of lipodermatosclerosis (C4) and an attempt to counteract the interstitial hypertension. Fibrous tissue further distorts the microcirculation and amplifies the ischemic obstructive condition which causes tissue destruction leading to skin ulceration. Lipodermatosclerosis is the hallmark of chronic venous insufficiency.
The skin and muscle vascular network of the distal gaiter region is a poor reservoir of pressure dissipation. Gravitational and obesity related venous hypertension, as well as venous shock from increased intra-abdominal pressure stress and retrograde venous shock under the muscle-venous pump of the calf cannot be absorbed by the reduced volume of the skin and muscular network of the distal gaiter region. Although the hydrostatic pressure is maximal at the plantar level, the volume of the microcirculation in this region with its rich muscle-cutaneous network provides sufficient dissipative capacity and adequate protection against venous hypertension. This may explain the absence of venous ulcers in this area.
Varicose ulcers are clinically distinct from venous ulcers. They develop at a point beneath the lowest point of the varicose veins and they usually have a small area. The adjacent skin is almost clinically normal. In many cases the gaiter region is likewise clinically normal and the ulceration may develop outside the usual gaiter area typical of the classical site of venous ulceration.
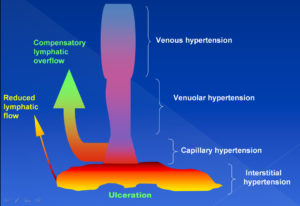
Venous hypertension exerts its effect on at least 4 levels (veins, venules, capillaries and the interstitial fluid).
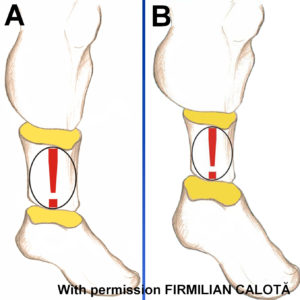
The clinical features of chronic venous insufficiency on tissue volume compared to a normal leg (A). The gaiter region is contracted (B) whilst the foot and upper calf are larger in volume (B).
Venous ulceration is not always in the gaiter region. It can be situated directly downstream of hidden (A) and more obvious varicose veins (B). These are termed varicose/variceal ulcers. Note the surrounding lipodermatosclerosis which is pathognomonic for venous ulceration.