The association between the presence of varicose veins and leg pain is very unclear. Varicose veins are common and do not bother many people. Leg pains are even more common and are frequently unrelated to varicose veins. There are many causes of leg pain. However, if their description contains a reference to feelings of heavy, weighty or swollen legs, the symptoms will most likely be of venous origin with very few remaining alternative diagnoses. If varicose veins are present the patient and doctor may attribute these pains to the varicose veins themselves or the underlying venous insufficiency. Recently, patients with venous symptoms but without venous disease or other causes of leg pain have been termed C0,s disease. Reconciling symptoms with pathology is a grossly neglected area of research.
WERNER BLӒTTLER Venous-type leg symptoms combine pain or mere discomfort with feelings of leg volume increase. They occur intermittently in normal, healthy individuals and carriers of varicose veins alike. Typically, symptoms involve both legs, increase along the day and in a warm environment, and cease with walking. The pathophysiology remains speculative. Perhaps it is the stretch of vein walls that activate pain receptors, the release of inflammatory cytokines in response to prolonged venous stasis. Perhaps it is caused by the prolonged loading of joints or other musculoskeletal reasons.
We examined the relationship between patients with varicose veins and compared them to healthy controls. Interestingly, the patients had a higher prevalence and greater severity of unrelated symptoms like headache and lower back pain. This was in addition to the higher prevalence and greater severity of leg symptoms like tingling, weakness and heaviness.
Furthermore, the prevalence of somatic and psychic symptoms in female patients presenting with “vein symptoms” but without any venous signs or other diagnosis was very high, between 54-88%. Somatic symptoms included tiredness, sleep disturbance and backache. Psychic symptoms included hypochondria, anxiety, depression, loss of vitality, impatience and feelings of inadequacy.
Venous symptoms should be seen as a self standing clinical entity as well as related to venous disease and a psychiatric predisposition.
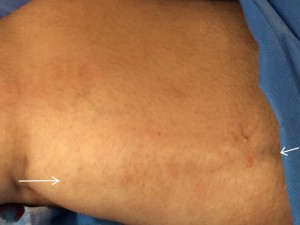
Post-inflammatory hyperpigmentation (PIH) along the course of a refluxing GSV (arrows from knee to groin). Although this is a common finding in patients with reflux it does not seem to be related to saphenous pain.