A common clinical dilemma is the management of patients with symptomatic varicose veins who have had a past deep vein thrombosis (DVT). In these cases it is unclear as to whether symptoms result from the post-thrombotic syndrome (PTS) or from superficial venous reflux/insufficiency (SVI), or a combination of both. If a DVT history is extracted from the patient or duplex ultrasound has identified deep venous disease, then there is controversy as to whether the superficial vein reflux should be treated to alleviate symptoms, or whether it should be left alone because of their perceived function as a collateral drainage pathway. In these circumstances a reliable test is required to establish the relative importance of the function of the superficial veins regarding beneficial collateral drainage versus detrimental reflux. One method has been proposed, below.
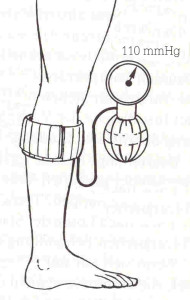
IMRE BIHARI We have developed a test for the patency of the deep subfascial collateral veins in patients with deep venous occlusion. We select patients with deep venous disease for removal of their varicose veins based on a simple haemodynamic test using a pneumatic tensiometer cuff. The cuff is placed around the limb just below or above the knee and inflated to a pressure of 110 mmHg. The patients are then asked to walk quickly for 5 minutes. In positive cases, the limb develops a bluish discolouration and the patient complains of intense pain whilst walking for 1-2 minutes. This implies that the deep veins are occluded and the superficial veins are compressed by the cuff, and there is no channel to drain the venous blood from the limb. In negative cases, when deep collateral channels in the subfascial space are sufficient in number and diameter to drain the venous blood from the leg, patients informed us that their legs felt better. This assumes that the cuff acts by occluding the superficial reflux selectively, thereby improving drainage, whilst maintaining the deep venous collaterals. In these cases we have performed superficial venous surgery with symptom relief and without compromising the venous return of the leg.
A tensiometer cuff is applied on the leg and inflated to 110 mmHg. The patient is then requested to walk for 5 minutes and record his symptoms.
As the patient walks, the calf muscle pump ejects the venous blood from the leg through collateral channels. If the deep subfascial collateral pathways are adequate then removal of the superficial refluxing veins is likely to improve symptoms. A, the cuff obstructs the superficial venous drainage. On walking, B-E, venous return is via deep collaterals.