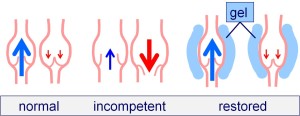
Vein dilatation is considered the primary event in patients with varicose veins, with valve incompetence as a consequence. The great saphenous vein (GSV) is usually affected. The resulting reflux can pressurise tributaries which drain into the GSV. This leads to dilatation and tortuosity detectable clinically as varicose veins. The treatment approach by most phlebologists is destructive, with an ablation or stripping procedure on the GSV. Restoration of competency has been achieved with a variety of techniques which include wrapping the valve regions with a cuff or spiral, valve suture and wall plication. However, these are invasive requiring a surgical wound. Occasionally, endovenous ablation techniques “fail” in their task in destroying the vein but cause a reduction in calibre with restoration of competency. This is unintentional but may lead to a preferable outcome. Percutaneous valvuloplasty is a recent innovation which focuses on the primary pathology by restoring the GSV to its normal calibre. This is achieved by filling the saphenous compartment in the region of the valve stations.
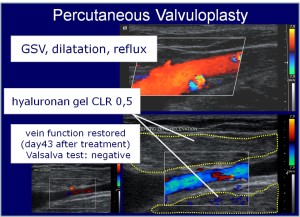
CHRIS RAGG We have been developing innovations in venous medicine for over 15 years and are currently perfecting the technique of percutaneous valvuloplasty, detailed on our website. Eligible patients must have preserved valve structures which are mobile. The injection of the gel is similar to the technique of tumescent anaesthesia but on this occasion it is used to support the valve structures and reduce the calibre of the vein. The dilated valve zones are shaped using perivenous injections of hyaluronan gel under ultrasound guidance. The viscosity of the gel has been improved using cross-linking and the inclusion of spherical particles of about 1 mm diameter. This allows for more precise gel deposition, preventing dispersion and adding support, thereby facilitating the shaping technique.
In 2014, a pilot study was performed in 20 patients with proximal GSV valve incompetence using percutaneous valvuloplasty. Antegrade flow, without reflux, was achieved in 19/20 cases and maintained over a one year period. Further injections were required 6/19 cases to maintain competency. There were no complications and no signs of relevant migration.
Future research will examine the effect of restoring GSV competency on its tributaries and on varicose vein recurrence. A clinical multicenter study using percutaneous valvuloplasty has been set up to examine the durability of this innovation.
Restoration of competency by shaping and supporting the valve station
Duplex ultrasound demonstrating the effect of percutaneous valvuloplasty at transforming a refluxive vein (top) into a competent vein (bottom left). Sufficient gel has been deployed to shape the valve station without compromising the lumen (bottom right).