Chronic venous obstruction (CVO) is a term used to describe venous obstruction related mostly to a previous deep vein thrombosis (DVT). Post-thrombotic changes occur in the form of fibrosis and scarring within deep veins. In some cases CVO can be caused by congenital abnormalities like vein aplasia, hypoplasia or agenesis. Occasionally, chronic mechanical obstruction is related to the external compression by benign lesions, including May-Thurner syndrome. Malignant masses or involved lymph nodes may also be responsible. Imaging studies usually reveal various local pathologies from a mild stenosis up to a total occlusion of the vein. The resulting impairment of drainage from the leg usually depends on the degree of collateral blood flow which can be worsened by reflux from concomitant valve destruction.
Whilst reflux is relatively easy to measure with duplex, plethysmography or descending venography, CVO is much more difficult to assess. Clinically, in most cases, CVO is recognized by the development of the post-thrombotic syndrome (PTS) which can include oedema, varicose veins or trophic skin changes. In the more severe cases venous claudication and ulceration can be observed.
TOMASZ URBANEK The outcome of DVT is unpredictable. Complete vein lumen recanalisation will occur in only 15-30% patients. The time required for a complete resolution of the venous thrombus is approximately 6 months. After 6 months the intra-luminal post-thrombotic changes are unlikely to resolve or change. No single non-invasive or invasive examination can properly detect borderline obstruction of potential haemodynamic importance. Current diagnosis is based mostly on the evaluation of clinical signs and symptoms as well as imaging studies including magnetic resonance venography (MRV), CT venography (CTV) or ascending contrast phlebography. Recently, the usefulness of intravascular ultrasound (IVUS) is also emphasized and may be the gold standard test according to several enthusiasts.
In patients with severe venous disease related to proximal CVO, venous stenting incurs a high technical success rate (84-93%) with satisfactory long term patency. Secondary patency rates approach 86% at 6 years in patients with post-thrombotic CVO. In patients with more distal CVO, conservative treatment methods are mostly implemented, especially compression stockings.
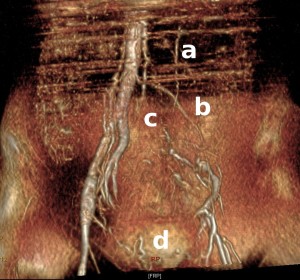
Magnetic resonance venogram (MRV) with post-thrombotic obstruction of the left iliac vein 3 years after a DVT. The left leg is drained by (a) gonadal, (b) mesenteric, (c) lumbar and (d) supra-pubic collaterals.